Highlights from the 90th European Atherosclerosis Society (EAS) Congress
Highlights from the 90th European Atherosclerosis Society (EAS) Congress
Milan, Italy saw the latest annual congress of the EAS which took place May 22-25, 2022. The meeting brought together many world-leading experts, academics, and clinicians with a special interest in the field of atherosclerosis and related vascular disease. The rich scientific programme offered novel insights in the therapy area, and how these may impact clinical guidelines for diagnosis and treatment of atherosclerotic cardiovascular disease (ASCVD). Some highlights of the congress are summarised below, particularly in relation to the role of diet and lifestyle in ASCVD risk management.
Opening the proceedings, EAS president Professor Kausik Ray reminded everyone of the importance of ongoing research, education, investment and interest in the field of CVD prevention. Approximately 2,300 delegates registered to attend the 2022 congress either in person or virtually, from across Europe and further afield.
Personalised ASCVD prevention: what does the future offer?
Novel developments in personalised approaches to atherosclerotic cardiovascular disease (ASCVD) prevention were presented. Dr Chiara Giannarelli highlighted the need to identify new therapeutic targets relevant to human disease, and the potential of deep phenotyping to delivery personalised therapies for ASCVD prevention. These in-depth studies of human samples to investigate plaque characteristics could unlock the door to application of precision medicine.(1)
Dr Eicke Latz presented evidence around lifestyle-associated triggers of ASCVD development. He described how inflammasomes play a critical role in regulation of inflammation and how via animal models it was demonstrated that the Western diet altered innate immune responses.(2) The NLRP3 inflammasome may have a crucial role in both the systemic response to Western diet exposure and in mediation of reprogramming.
According to Professor Wolfgang Koenig, new findings support the role of multimodal imaging along with traditional biomarkers to identify atherosclerotic plaque in clinical settings to evaluate disease endpoints. He outlined how biomarkers of vascular inflammation have been shown to enhance risk assessment and targeting of therapy in secondary prevention(3,4) and how targeted plasma proteomics together with machine learning techniques model may outperform clinical risk factors in predicting CVD risk in primary prevention.(5,6)
Dr Amit Khera discussed the potential of genetic risk scores; how genome interpretation has come a long way and could be used alongside traditional risk factor assessment criteria a for the delivery of precision ASCVD prevention. Polygenic risk scores may offer risk stratification early in life before the onset of traditional risk factors, and thus the opportunity to intervene early with lifestyle and drug therapy to significantly reduce CVD risk.(7) Dr Khera recognised the important health opportunity of identifying those with high inherited risk who can benefit from early intervention to improve their lifetime CVD risk.(8)
A tool for implementation of a healthy diet
Promising findings suggest the incorporation of a short dietary assessment into ten-year absolute risk calculations may help motivate patients to adhere to dietary guideline recommendations and advance personalised prevention.(9)
In a study of 94,321 individuals from the Copenhagen General Population Study, Emilie Westerlin Kjeldsen, Professor Ruth Frikke-Schmidt and colleagues investigated the impact of incorporating dietary assessment (short and valid food frequency questionnaire) into ten-year absolute risk estimates for CVD.(9) The authors postulate that the dietary assessment may enhance motivation patients to make dietary improvements, since this could be easier to translate to positive behaviour change compared to other risk factors such as cholesterol and blood pressure. Poor dietary patterns remain one of the major modifiable risk factors for CVD due to their association with dyslipidemia and ASCVD development so this new tool could be an exciting development to unlock a more personalised approach to encourage individuals to change and maintain healthy diets are lacking.
Prevention guidelines with focus on dyslipidemia
Professor Ian Graham talked about advances in current risk estimation tools used in dyslipidemia guidelines. He flagged the limitations of the existing risk calculation systems including the fact that estimation systems apply to populations, not individuals and focus on fatal CVD only, over a rather narrow and late age range of 40-65 years. Most estimates of lifetime risk start at about age of 40 which is about 40 years too late especially given the growing understanding of early life determinants and genetics for example. He emphasised that more early identification of risk is needed and that combining genetic estimates and other novel factors may help deliver a more personalised approach to risk estimation.
A compelling session delivered by Dr Brian Ference detailed what was new and noteworthy about the 2021 ESC guidelines on cardiovascular disease prevention in clinical practice, particularly regarding risk prediction due to risk and benefit estimation. He recapped the importance of having the clear declarative statement that LDL-cholesterol causes atherosclerosis beyond all doubt, and the benefit of lowering LDL depends on both the magnitude and the duration of exposure. LDL-cholesterol is not only the main cause of atherosclerotic CVD, but it causes accumulating injury to the arterial wall over time and therefore has a cumulative effect.(10-12) Ference critiqued the approach of current risk calculators and guidelines which determine intervention and management strategies based on 10-year risk of CVD events when the evidence clearly states it’s lifetime exposure that matters. The algorithms are such that once someone has a high 10 year risk they likely already have developed an atherosclerotic plaque burden and at this point can’t benefit to the same extent from prolonged risk reduction that may have been possible earlier in life. Ference suggested that optimal opportunities for intervention exist when there is asymptomatic plaque progression early in life before the long-term exposure to LDL-cholesterol.(11) Although lifetime risk calculators could hold potential, there are mathematical shortfalls in the QRISK and JBS3 (the basis of the 2021 ESC lifetime risk calculator) which systematically underestimate the magnitude of the effect of the known modifiable causes of ASCVD events, particularly LDL-C and blood pressure.(13)
Professor Michal Vrablík spoke about the implementation of a personalised approach to CVD prevention and concluded that though often difficult to implement, it is necessary in day-today clinical practice. He urged healthcare practitioners to help reduce non-adherence to interventions and minimise therapeutic inertia. He also supported to role of lifestyle changes no matter the patients age and proposed that the strategy of pharmacological treatment should be combination.
Environment and cardiovascular risk
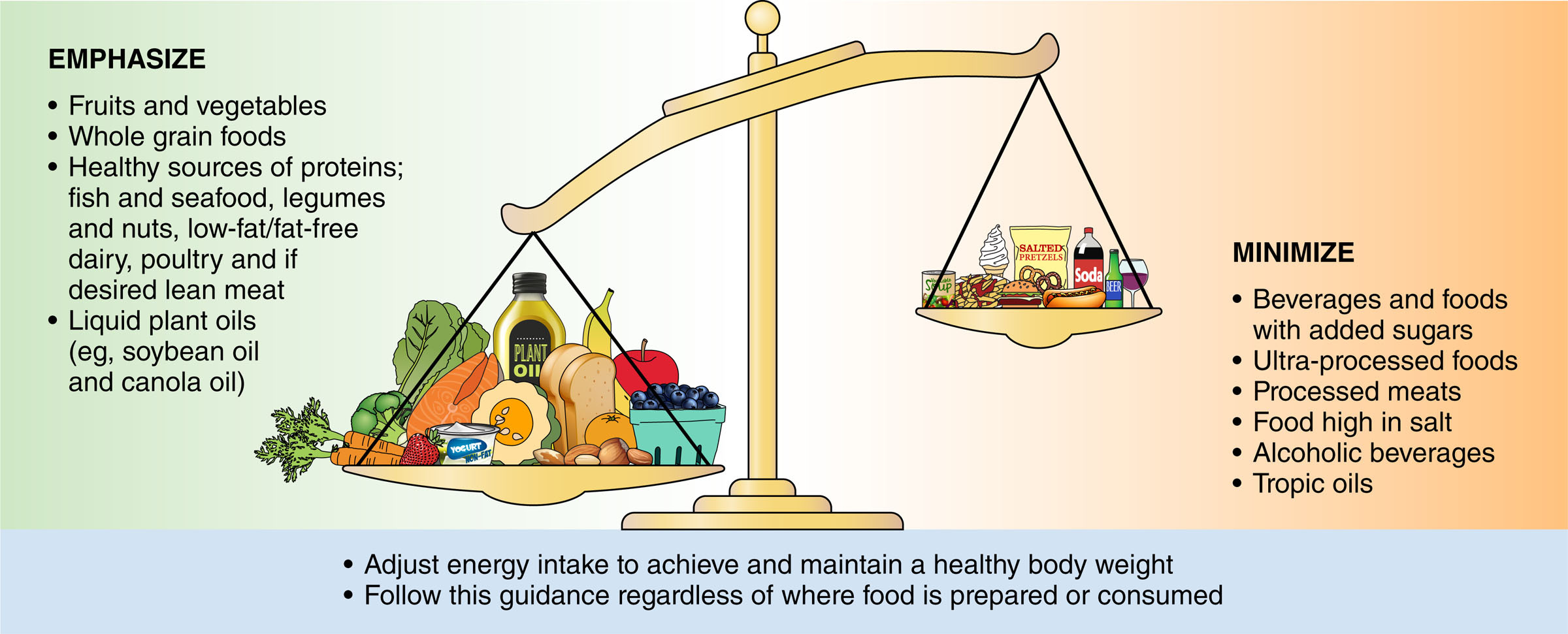
Dr Alice Lichtenstein eloquently summarised the ways in which dietary components and patterns are determinants of cardiovascular risk. She re-emphasised what is well understood about diet being the major risk factor of coronary heart disease, alongside those risk factors directly related to diet (high blood pressure, cholesterol and fasting blood glucose).(14) Dr Lichtenstein flagged the impact of whole diet, not just one component and referenced the most recent dietary guidance form the American Heart Association including the 10 features of evidence-based dietary guidance to promote cardiovascular health summarised below:(15)
1. Adjust energy intake and expenditure to achieve and maintain a healthy body weight
2. Eat plenty of fruits and vegetables, choose a wide variety
3. Choose foods made mostly with whole grains rather than refined grains
4. Choose healthy sources of protein
a. mostly protein from plants (legumes and nuts)
b. fish and seafood
c. low-fat or fat-free dairy products instead of full-fat dairy products
d. if meat or poultry are desired, choose lean cuts and avoid processed forms
5. Use liquid plant oils rather than tropical oils (coconut, palm, and palm kernel), animal fats (e.g. butter and lard), and partially hydrogenated fats
6. Choose minimally processed foods instead of ultra-processed foods
7. Minimize intake of beverages and foods with added sugars
8. Choose and prepare foods with little or no salt
9. If you do not drink alcohol, do not start; if you choose to drink alcohol, limit intake
10. Adhere to this guidance regardless of where food is prepared or consumed
Dr Lichtenstein concluded that we need creative approaches to promote improvements in dietary patterns and focus on whole diet and not single nutrients. She suggested we work to improve the default options in our diets and unify current guidance.
Professor Patrick Schrauwen discussed the role of exercise: ‘When, how and who?’. He reminded us that there is little doubt about the benefits of exercise for all around good health and the established role of exercise reducing fat in and around the heart and thus improving cardiovascular function.(16) Schrauwen described how one study suggested afternoon training may be more beneficial to metabolic health than exercise at other times of day(17) and further research concluded that increasing standing and walking had a major improvement on circulating lipids and insulin sensitivity.(18,19)
Tess Yntema took the audience through how gut microbiota dysbiosis has been linked to CVD.(20) She provided an overview of emerging evidence from mice models of the role of commensal bacteria in protecting against atherosclerosis. Microbial production of short-chain fatty acids potentially contribute to the athero-protective effect.(data unpublished)
Paediatrician Dr David Burgner reminded the congress audience of the accrual of CVD risk across lifecourse, flagging the preventable aspects especially in early life and highlighting the understanding that inflammation is key to pathogenesis.(21) He made a strong case for the fact that health status in early life can help determine later life risk of disease, detailing the link between childhood infection with later CVD due mainly to variable but considerable mediation by inflammation.
Primordial prevention: The neglected topic
Dr Kevin Maki delivered an excellent talk entitled “What is the optimal diet to prevent ASCVD?”. Dr Maki reminded us that primordial prevention is aimed at preventing the development of risk factors, compared to primary prevention which relates to CVD events further down the road.(22) The benefits of primordial prevention include a greater reach and larger potential benefit at a population level. Resource requirements for treatment are dramatically higher than addressing the root causes earlier on.(22) He stressed the importance of lifetime risk reduction given what we know about prolonged risk exposure e.g. 1 mmol/L lower level of LDL-C over roughly 5 years is associated with a 22% lower risk of a CVD event.(23) Longer prospective cohorts indicate the same LDL-lowering is associated with a 52% lower risk of CVD. Dr Maki stressed that lower LDL-cholesterol for longer is better, and modest reductions in risk (e.g. less than 0.4 mmol/L LDL-C reduction), if maintained for longer periods of time, can have a dramatic impact on risk for ASCVD events.
Dr Maki stated that lifestyle is the cornerstone of primordial prevention and within that diet plays a substantial role, stressing that an adequate nutritional intervention in a developmental critical period can change the outcome from childhood into adulthood. He referenced the 2021 ESC guidelines on CVD prevention in clinical practice(10) and the ASA 2021 Dietary Guidance to Improve Cardiovascular Health(15) regarding dietary recommendations in practice. Maki concluded that promoting a healthy diet and lifestyle from early life is optimal for avoidance of adverse CVD outcomes because ASCVD starts early and is progressive over decades.
Recommendations for nutrition and alcohol from the 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice(10)
| Recommendations | Class* | Level** |
| A healthy diet is recommended as a cornerstone of CVD prevention in all individuals. | I | A |
| It is recommended to adopt a Mediterranean or similar diet to lower risk of CVD. | I | A |
| It is recommended to replace saturated with unsaturated fats to lower the risk of CVD. | I | A |
| It is recommended to reduce salt intake to lower BP and risk of CVD | I | A |
| It is recommended to choose a more plant-based food pattern, rich in fibre, that includes whole grains, fruits, vegetables, pulses, and nuts | I | B |
| It is recommended to restrict alcohol consumption to a maximum of 100 g per week | I | B |
| It is recommended to eat fish, preferably fatty, at least once a week and restrict (processed) meat. | I | B |
| It is recommended to restrict free sugar consumption, in particular sugar-sweetened beverages, to a maximum of 10% of energy intake. | I | B |
* Class of recommendation. (I= Evidence and/or general agreement that a given treatment or procedure is beneficial, useful, effective)
** Level of evidence. (A= Data derived from multiple randomized clinical trials or meta-analyses, B= Data derived from a single randomized clinical trial or large non-randomized studies)
Evidence-based guidance for dietary patterns to promote cardiovascular health from the ASA 2021 Dietary Guidance to Improve Cardiovascular Health(15)
References
(1) Pasterkamp G, den Ruijter, Giannarelli. Arterioscler Thromb Vasc Biol 2022; 42: e86-e95.
(2) Latz E. Nat Rev Immunol 2021; 21: 622-623.
(3) Ford I, et al. J Am Coll Cardiol 2016; 68: 2719-2728.
(4) Antonopoulos AS, et al. JACC Cardiovasc Imaging 2022; 15: 460-471.
(5) Hoogeveen RM, et al. Eur Heart J 2020; 41: 3998-4007.
(6) Nurmohamed NS, et al. Eur Heart J 2022; 43: 1569-1577.
(7) Khera AV, Kathiresan S. Circulation 2017; 135: 1005-1007.
(8) Fahed AC, Philippakis AA and Khera AV. Nat Commun 2022; 13(1): 2922.
(9) Kjeldsen EW, et al. Lancet Reg Health Eur 2022; 19: 100419.
(10) Visseren FLJ, et al. Eur Heart J 2021; 42(34): 3227-3337.
(11) Ference BA, et al. Eur Heart J 2020; 41(24): 2313-2330.
(12) Mach F, et al. Eur Heart J 2020; 41(1): 111-188.
(13) Hippisley-Cox, et al. BMJ 2010; 341: c6624.
(14) Dai H, et al. Eur Heart J Qual Care Clin Outcomes 2022; 8(1): 50-60.
(15) Lichtenstein AH, et al. Circulation 2021; 144: e472–e487.
(16) Schrauwen-Hinderling VB, et al. J Clin Endocrinol Metab 2010; 95(4): 1932-8.
(17) Mancilla R, et al. Physiol Rep 2021; 8(24): e14669.
(18) Duvivier BMFM, et.al. Front Physiol 2017; 8: 353.
(19) Remie CME, et.al. Diabetologia 2021; 64(12): 2817–2828.
(20) Karlsson F, et al. Nat Commun 2012; 3: 1245.
(21) Bekkering S, et al. Trends Endocrinol Metab 2020; 31(5): 378-389.
(22) Capra ME, et al. Nutrients 2021; 13(7): 2359.
(23) Ference BA, et al. Eur Heart J 2017; 38(32): 2459-2472.
